Discover How Long It Takes for Mirena to Stop Periods: A Comprehensive Guide for 2025
Discover How Long It Takes for Mirena to Stop Periods: A Comprehensive Guide for 2025
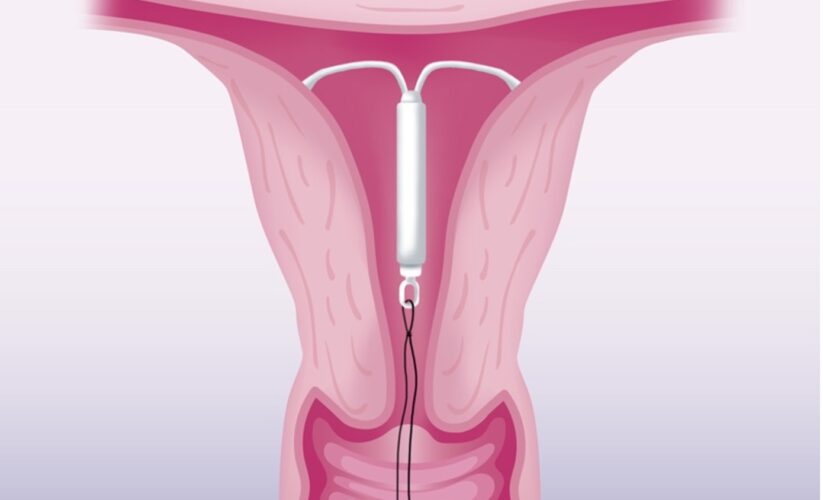
Mirena, a popular intrauterine device (IUD), has garnered attention for its ability to provide effective contraception while also influencing menstrual cycles. Many women often ask, “How long does it take for Mirena to stop periods?” This article delves into the details surrounding Mirena’s impact on menstrual cycles, including user experiences, hormonal effects, and the key considerations for individuals contemplating its use.
Understanding Mirena and Its Functions
Mirena is a hormonal IUD that releases levonorgestrel, a synthetic progesterone, directly into the uterus. This hormone plays a crucial role in modifying the body’s monthly menstrual cycle by thickening cervical mucus and thinning the uterine lining, which helps in preventing pregnancy and often leads to lighter periods. However, many women consider Mirena not only for its contraceptive efficacy but also for its potential to stop periods altogether. Typically, users report a significant reduction in menstrual flow within the first three to six months of use. By the end of the first year, many find that their periods have ceased altogether or have become minimal.
What to Expect After Mirena Insertion
After getting the Mirena IUD inserted, women may experience various changes due to hormonal adjustments. It’s common to have irregular bleeding, especially in the initial months following insertion. While some may find their periods stopping entirely, bleeding patterns can vary greatly. Users often report a significant drop in flow, with many experiencing just spotting rather than full menstrual bleeding. This initial unpredictability can be concerning, so consulting with a healthcare provider is advisable for personalized insights into one’s experience with Mirena.
Mirena’s Effectiveness Timeline
The effectiveness of Mirena in stopping periods generally follows a predictable timeline. Originally, the device provides substantial contraceptive protection immediately upon insertion if done during the first seven days of the menstrual cycle. Many users begin to notice changes in their cycle within approximately three months, with average cessation of menstrual bleeding observable by the six-month mark. Although some individuals might take longer to experience a complete halt in menstruation, consistent and long-term use typically offers greater satisfaction regarding period cessation.
User Experiences and Reviews
User experiences with Mirena can relate directly to its effectiveness in stopping periods. Numerous testimonials highlight significant benefits for managing heavy periods and reducing the total number of menstrual days. For instance, many women appreciate the transition to lighter bleeding or amenorrhea (the absence of menstruation) as a positive outcome of using Mirena. However, it’s equally essential to note reports of side effects, such as mood changes, weight fluctuations, or irregular bleeding patterns. Engaging in Mirena support groups can provide reassurance and understanding, allowing new users to gauge the varied experiences of others.
Mirena and Hormonal Effects on Menstruation
The hormonal effects of Mirena go beyond mere contraception; many users note significant changes in their menstrual cycles. As Mirena releases levonorgestrel, users experience alterations in their bleeding patterns—a combination of lighter periods, reduced cramping, and, eventually, absence of periods altogether. Understanding these effects assists users in managing expectations following insertion.
Mirena and Mood Changes: What to Consider
One common concern when it comes to hormonal contraceptives, including Mirena, is mood stability. Some women report fluctuations in emotional well-being during the first months post-insertion. It’s crucial to distinguish between normal adjustment periods and significant mood alterations that may warrant a discussion with healthcare providers. Migration to a hormonal method like Mirena should be routinely monitored for emotional shifts, especially in those with prior mood disorder histories.
Effects on Fertility and Cycle Regulation
When considering Mirena as a long-term option, understanding its effects on future fertility is critical. Most studies indicate that normal fertility usually resumes shortly after the removal of Mirena in cases where women wish to conceive. The device’s impact also promotes cycle regulation during its use, making it beneficial for women with irregular menstrual cycles or conditions such as endometriosis.
The Safety Profile of Mirena
Mirena’s safety profile is generally strong, with low rates of major complications. Like many hormonal contraceptives, potential side effects such as irregular bleeding or hormonal imbalances may occur but are often transient. Open conversations with a healthcare provider can elucidate personal risks and help mitigate any concerns regarding the safety and effectiveness of the Mirena IUD.
Practical Tips for Managing Period Changes with Mirena
Successfully navigating period changes with Mirena requires a combination of patience and proper management strategies. Women should be aware of common side effects and how to adapt their self-care routines post-insertion.
Managing Initial Bleeding Patterns
In the months following insertion, irregular bleeding can become a norm as the body adjusts to Mirena’s hormonal influence. Patients should track their cycles noting changes to discuss with their healthcare provider. Utilizing menstrual tracking apps can help in managing expectations, forecast menstrual phases, and monitor any concerning irregularities regarding bleeding.
Communicating with Healthcare Providers
Regular follow-up care with a healthcare provider is pivotal in managing the transition to Mirena. Discussions about bleeding patterns, side effects, and overall satisfaction can help shape a tailored approach to further contraceptive method usage or transition strategies if necessary. Furthermore, arranging regular checkups post-insertion can help ensure the IUD remains properly positioned and effective.
Engaging with Support Groups and Online Communities
Connecting with others who have shared similar experiences can offer emotional support and practical tips on navigating Mirena’s impacts on periods. Many online groups provide platforms for sharing insights regarding Mirena’s side effects, long-term effectiveness, and personal stories regarding whether they found success in halting periods. This communal sharing can bolster confidence for prospective users unsure about their choice.
Key Takeaways
- Many users notice a reduction in menstrual flow within three to six months of Mirena insertion.
- Mirena can often lead to lighter periods or complete cessation, depending on individual hormonal responses.
- Patients should maintain open communication with their healthcare providers regarding any changes or side effects experienced with Mirena.
- Engaging with support communities can provide valuable insights and feedback on personal experiences and outcomes with Mirena.
FAQ
1. How can Mirena affect my overall menstrual health?
Mirena significantly alters menstruation by regulating the menstrual cycle, leading to lighter periods or complete amenorrhea in many users. Engaging with a healthcare provider can illuminate potential impacts on menstrual health tailored to individual needs.
2. What are the common reviews about Mirena after prolonged use?
Many women have favorable impressions of Mirena for its effectiveness in managing heavy periods and offering long-lasting contraception. However, some users also mention side effects, ranging from hormonal fluctuations to weight changes. Reading user testimonials can provide balanced insights.
3. How does placement differ from other contraceptive methods?
Mirena insertion requires a healthcare professional and typically involves a short appointment, differing from “at-home” methods like birth control pills. It’s crucial to understand the placement process, effectiveness, and individual health considerations before undergoing the procedure.
4. Can Mirena lead to weight gain?
Weight changes are possible with Mirena due to hormonal shifts affecting metabolism. However, individual responses vary; therefore, monitoring changes after insertion can provide patients with insights into their specific reactions to the device.
5. What should I do if I experience persistent irregular bleeding?
If you experience prolonged or heavy bleeding after the initial adjustment period, consulting your healthcare provider is advisable. They can assess the situation to determine if further interventions or examination are necessary.
6. Will my menstrual cycle return to normal after Mirena is removed?
Typically, menstrual cycles normalize soon after Mirena removal. However, the timeline may vary among individuals, so keeping in touch with a healthcare provider about expectations and experiences is essential.
7. How do I manage side effects from Mirena?
Managing side effects can involve regular discussions with healthcare providers regarding symptoms and potential solutions. Empowering oneself with knowledge through community interactions and professional guidance aids in navigating Mirena-related concerns effectively.